Anne Kerber, Senior Vice President, Head of Cell Therapy Development
Historically, in oncology clinical trials at Bristol Myers Squibb and industry-wide, success has been largely measured by one main endpoint: overall survival (OS). To meet this endpoint, development strategists look to "de-risk" trials by removing as many unknown variables as possible. This "de-risking" can include selecting overly uniform participant populations or delaying patients with rapidly progressing disease from accessing the investigative treatments.
While some de-risking is necessary, many of these strategies are at odds with ensuring clinical trials are truly patient-centric, meaning they are powered to identify medicines that will effectively treat diverse patient populations that reflect the real world.
At Bristol Myers Squibb, we are working to strike this complex balance as we evolve toward a new definition of success that better serves our patients. And there is, perhaps, no better place to implement this approach than clinical trials evaluating cell therapies, where the need for true patient-centricity is especially critical.
Achieving "success" redefined: Lessons from cell therapy clinical development
Traditionally, clinical trials investigating autologous cell therapies, which involve reengineering a patient's own cells into treatments, have been tightly controlled and restricted to specific patient populations, given the challenges and lengthy turnaround times of these personalized therapies. However, excluding patients from these trials due to aggressive disease or high tumor burden leads to biased enrollment not reflective of real-world patients.
Our Bristol Myers Squibb cell therapy development team is committed to combating these barriers to true patient-centricity by redesigning our clinical trials to meet a new standard of success.
For example, we designed our TRANSFORM Phase 3 clinical trial to allow enrollment of high-risk patients with relapsed or refractory large B-cell lymphoma (LBCL) by allowing bridging therapy and cross-over to provide rapidly progressing patients immediate access to our investigative chimeric antigen receptor (CAR) T cell therapy despite the potential negative impacts it may have on our key secondary endpoint of overall survival.
Encouragingly, these patient-centric measures were, in fact, not disruptive to our redefined definition of “success.” Despite a large proportion of patients receiving bridging therapy, which reflects clinical practice, study results showed a clinically meaningful benefit for patients enrolled with or without bridging therapy.
TRANSFORM was designed with an efficient sample size to enable early data readout while maintaining the statistical power and integrity of the highly patient-centric trial design.
Systematically incorporating patient and advocate voices drives patient-centricity
One fundamental way we’re making progress toward this evolved meaning of clinical and real-world “success” is by applying a patient-centric lens to every stage of clinical development. We do this by listening to what patients and their communities need and bringing their voices into our development process from the start.
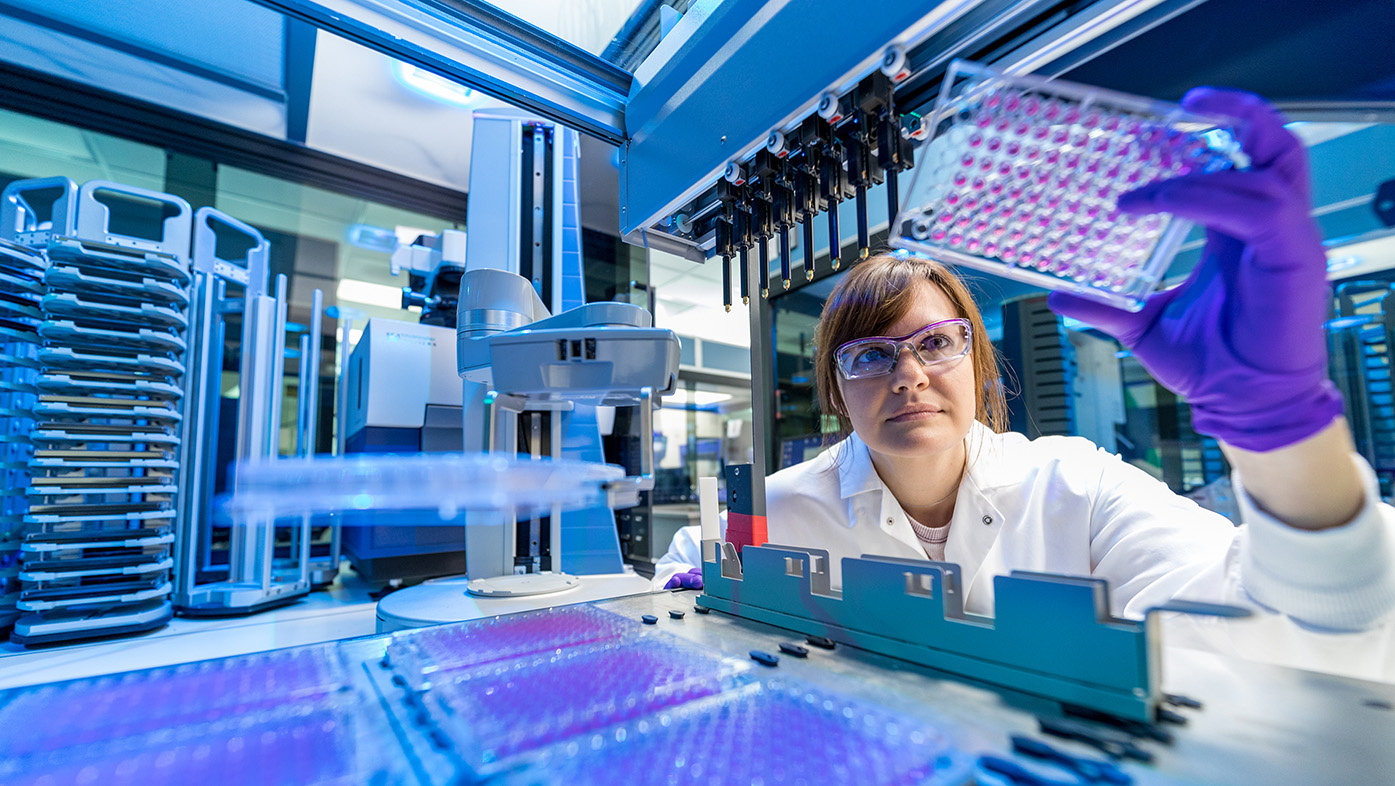
In 2020, Bristol Myers Squibb launched our Patient Expert Engagement Resource (PEER), one of the first programs of its kind, that partners with more than 80 patient advocacy groups to weave perspectives from patients worldwide into every step of drug discovery and development, including clinical trial design.
During early-stage development, PEER input guides our strategies like optimizing drug design and delivery to better serve patient needs. It also shapes our clinical trial development by adding more inclusive participant criteria, kinder and safer study design, and easier-to-understand data readout language.
In fact, since PEER launched, all clinical trial protocols across Bristol Myers Squibb are eligible to receive this patient and advocate input, and it is mandatory for all Phase III trials before moving forward. This allows us to be more confident that our therapies, if approved, will have the best opportunity to treat as many patients as possible and help eliminate geographical, racial, or social health equity disparities that come from underrepresented drug development programs.
Increased outreach is key to reaching our communities
We are also working with community partners on new outreach strategies to combat other patient-centric clinical trial barriers, including limited awareness around clinical trials and overall mistrust of the healthcare system. As part of this work, to date, we’ve awarded millions of dollars in health equity grants to 24 U.S. non-profit organizations that aim to improve access and quality care to medically underserved communities across a wide array of therapeutic areas.
Overall, I feel encouraged by the ways I’ve witnessed true patient-centricity seep into so many aspects of our work at Bristol Myers Squibb. By placing a holistic view of the patient in our clinical trial designs, backed by the real-life experiences of patients around the world, we’re redefining what success looks like not just for some but for all.
Similar to so many things in this industry, we must work together to ensure meaningful and lasting change. But at Bristol Myers Squibb, we do not shy away from challenges, and I am thrilled to work with and learn from my esteemed colleagues and peers to tackle those challenges every day.